Study ID’s Genetic Mutations Contributing to Adult Epilepsy
- johnshohfi
- May 26, 2023
- 3 min read
Original Article by Haley Bridger

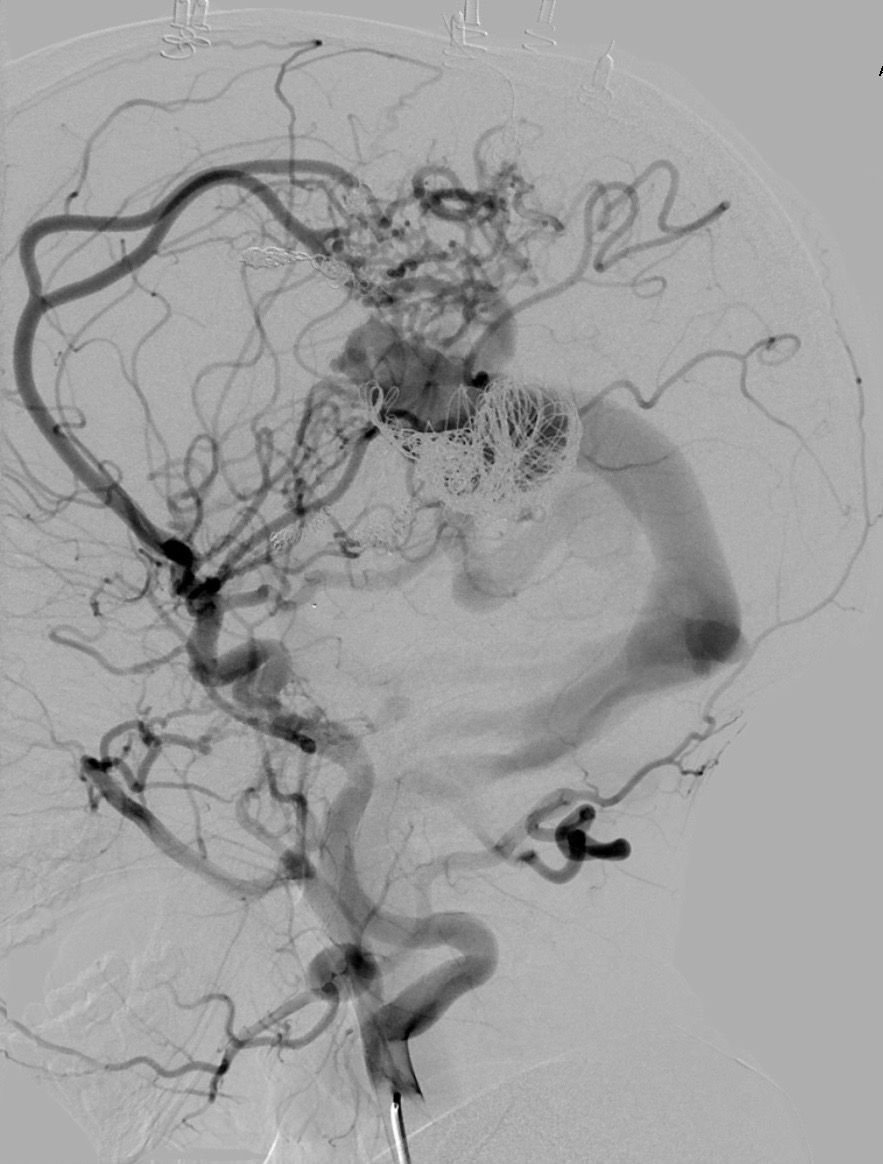
Epilepsy affects approximately 1-in-26 people and the most common form, known as temporal lobe epilepsy (TLE), often cannot be adequately treated with anti-seizure medications. Patients with this form of epilepsy may require neurosurgery to provide relief from seizures.
The condition’s origins and progression are not well understood, and it has been unclear if genetic mutations may contribute to TLE.
A new study by Harvard Medical School investigators at Brigham and Women’s and Massachusetts General hospitals, in collaboration with colleagues at Boston Children’s Hospital, sheds new light on the role of somatic mutations in TLE — DNA alterations that occur after conception — and suggests the potential of using existing cancer therapies to treat TLE that is resistant to anti-seizure medications. The results are published in JAMA Neurology.
“Somatic mutations are likely an underappreciated and significant cause of neurologic diseases, particularly for epilepsy,” said co-first author Sattar Khoshkhoo, HMS instructor in neurology at Brigham and Women’s Hospital.
“And as an epileptologist who specifically focuses on epilepsy genetics in my clinical practice, my underlying assumption is that all epilepsy is due to genetic causes until proven otherwise. We are discovering more and more new genetic pathways in epilepsy, which is important because our goal is to offer more specific, targeted treatments for individual patients and offer guidance on who would benefit from one treatment versus the other,” he said.
“Our results provide the first solid insight into this most common form of adult epilepsy,” said co-senior author Christopher A. Walsh, the Bullard Professor of Pediatrics and Neurology at Boston Children’s Hospital.
“It shows that epilepsies that are not usually inherited can still be genetic in their mechanism. And the specific genetic pathway we have identified, RAS/MAPK, opens a whole new avenue of therapeutic possibilities, since anti-cancer drugs that target this pathway may have unexpected uses in epilepsy,” Walsh said.
To uncover somatic mutations, Khoshkhoo and colleagues performed a case-control genetic association study, analyzing DNA from brain tissue samples collected from 105 patients with epilepsy and 30 controls between 1988 and 2019.
The team sequenced portions of the genome coding for proteins (whole exome sequencing) and looked at specific locations in the genome (gene-panel sequencing), with each genomic region sequenced more than 500 times on average.
The team pinpointed 11 somatic mutations that were enriched in hippocampus, the region of the brain where seizures typically originate, from 11 patients with treatment resistant TLE. All but one of the 11 mutations were connected to a specific genetic pathway known as the RAS/MAPK pathway.
This finding is particularly important because several anti-cancer drugs have been developed to target the RAS/MAPK pathway. If the study’s results are confirmed and validated, such drugs could be tested for the treatment of TLE.
In addition to suggesting a potential path to treatment, the findings could also be used to help inform treatment decisions for patients who do or do not harbor these somatic mutations.
“This work is exciting because it identifies potential drug targets that can be modulated with repurposed, FDA-approved anti-cancer agents. This suggests the potential for a rational, precision medicine treatment for a problem that we currently treat by removing a significant part of the temporal lobe with neurosurgery,” said Kristopher Kahle, the Nicholas T. Zervas Associate Professor of Neurosurgery at Harvard Medical School and chief of Pediatric Neurosurgery at Massachusetts General Hospital.
Kahle also holds research appointments in genetics/genomics and neurosurgery at Boston Children’s Hospital.
The authors noted that their study includes samples only from patients whose disease was severe enough to require surgery and may not be generalizable to patients with less severe disease.
In addition, samples from these patients may have more scarring and cell death from seizures. This could mean that the somatic mutations they detected may be much more prevalent than the rates found in this study.
The investigators plan to test a larger number of hippocampus samples and use cell models to test pre-existing drugs.
“Our findings point to the potential for developing the first disease modifying treatment in TLE,” said Khoshkhoo.
“Being able to provide a genetic diagnosis has implications for clinical decision making and could signal a new day for treatment.”



Comments